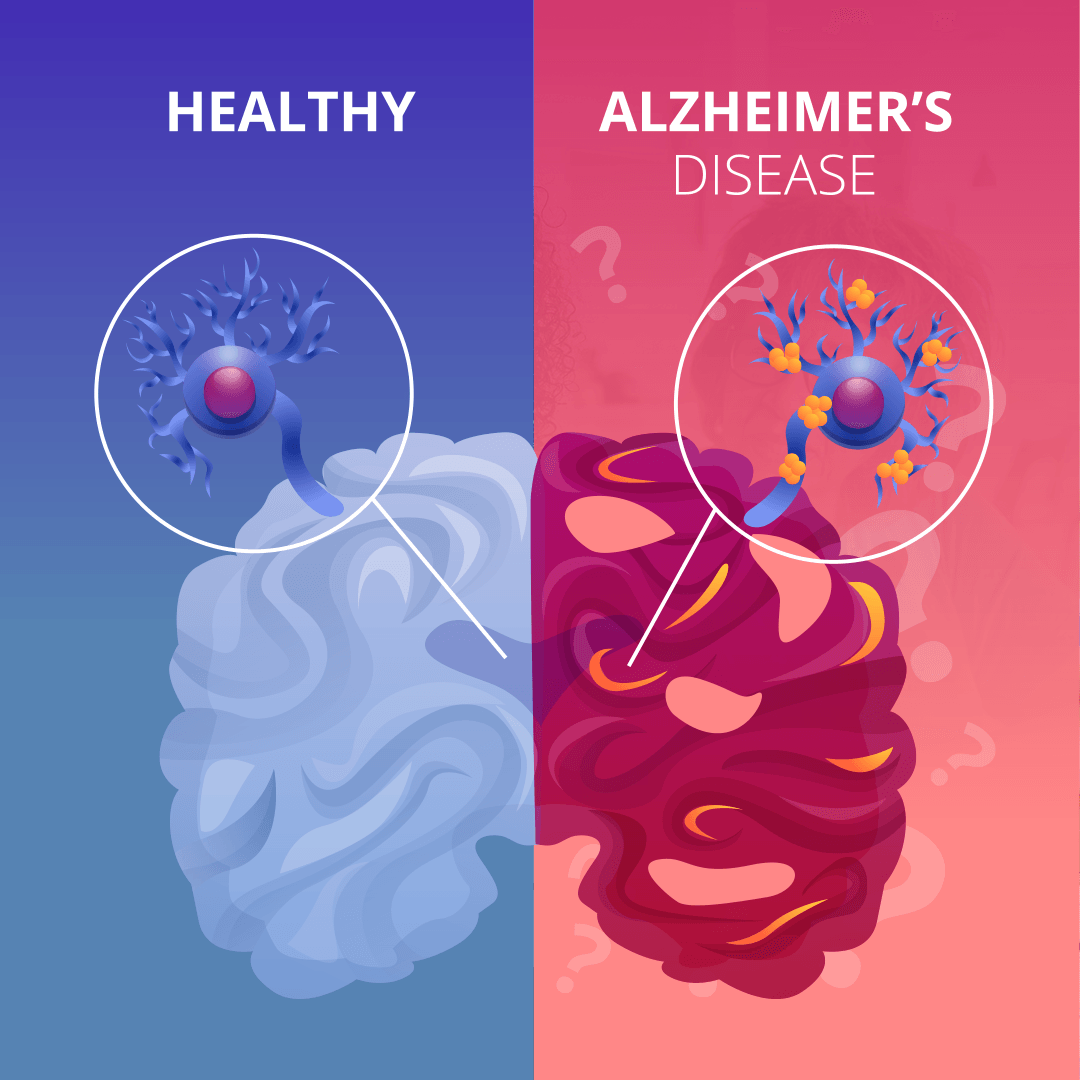
1. Introduction Alzheimer’s disease is a complex and devastating condition that affects millions of individuals worldwide. As healthcare professionals, it is essential to have a comprehensive understanding of this disease in order to provide the best possible care and support to patients and their families.. 2. What is Alzheimer’s Disease? Alzheimer’s disease is a progressive brain disorder that affects memory, thinking, and behavior. It is the most common cause of dementia, accounting for approximately 60-80% of all cases. This debilitating condition primarily affects older adults and gradually worsens over time. The exact cause of Alzheimer’s disease is still unknown, although researchers believe it may be a combination of genetic, environmental, and lifestyle factors. In Alzheimer’s disease, abnormal deposits of proteins form plaques and tangles in the brain, interfering with the communication between brain cells and ultimately causing their death. Early symptoms of Alzheimer’s disease often include mild forgetfulness and difficulty with problem-solving and language. As the disease progresses, individuals may experience confusion, disorientation, personality changes, and difficulty performing daily tasks. While there is currently no cure for Alzheimer’s disease, various treatment options are available to manage symptoms and improve quality of life. These may include medications to slow down the progression of the disease, behavior and lifestyle interventions, and supportive therapies such as cognitive rehabilitation. In the next section, we will delve deeper into the causes and risk factors associated with Alzheimer’s disease, shedding light on the latest research and advancements in understanding this complex condition. Stay tuned for more valuable insights into the world of Alzheimer’s disease! 3. Recognizing the signs and symptoms Recognizing the signs and symptoms of Alzheimer’s disease is crucial for timely intervention and support. While the earliest stages of the disease may present with subtle changes in memory and cognitive function, it is important for healthcare professionals to be vigilant in identifying these early warning signs. Common signs of Alzheimer’s disease include frequent forgetfulness, difficulty with problem-solving and decision-making, confusion in familiar environments, changes in personality and mood, and struggles with language and communication. These symptoms may also be accompanied by difficulty in completing familiar tasks and a general decline in cognitive abilities. By being aware of these indicators, healthcare professionals can facilitate early diagnosis and intervention, allowing for better management of the disease and improved quality of life for patients and their families. In the next section, we will explore the diagnostic process for Alzheimer’s disease, including the various assessment tools and techniques that healthcare professionals can utilize to accurately identify and evaluate the condition. Stay tuned for an informative discussion on this crucial aspect of Alzheimer’s disease management. 4. Diagnosing Alzheimer’s Disease In diagnosing Alzheimer’s disease, healthcare professionals utilize a combination of assessments and evaluations to accurately identify the condition. The process typically begins with a thorough medical history review and physical examination to rule out other potential causes of cognitive decline. One commonly used assessment tool is the Mini-Mental State Examination (MMSE), which evaluates cognitive function in areas such as memory, attention, and language. Another valuable tool is the Montreal Cognitive Assessment (MoCA), which assesses various cognitive domains including executive function, attention, and visuospatial abilities. In addition to these standardized tests, healthcare professionals may also consider brain imaging techniques such as magnetic resonance imaging (MRI) or positron emission tomography (PET) scans to assess brain structure and function. These imaging studies can help to identify changes in the brain associated with Alzheimer’s disease. By incorporating a comprehensive diagnostic approach, healthcare professionals can provide accurate diagnoses and develop appropriate treatment plans for individuals with Alzheimer’s disease. In the following section, we will explore the available treatment options and management strategies that can help improve the quality of life for those affected by this condition. Stay tuned for further practical insights into Alzheimer’s disease care. 5. Treatment options for Alzheimer’s Disease Once a healthcare professional has accurately diagnosed Alzheimer’s disease, it is crucial to develop a treatment plan tailored to the individual’s specific needs. While there is no cure for Alzheimer’s, various treatment approaches can help alleviate symptoms and slow down the progression of the disease. Pharmacological interventions are often used in the management of Alzheimer’s. Cholinesterase inhibitors, such as donepezil, rivastigmine, and galantamine, are commonly prescribed to improve cognitive function and help with memory loss. Another medication called memantine may also be used to regulate glutamate levels in the brain, which can help slow down cognitive decline. Non-pharmacological interventions are equally important and can include cognitive stimulation therapy, physical exercise, and occupational therapy. These approaches aim to enhance overall brain health, promote social interaction, and maintain independence for as long as possible. In the next blog section, we will explore these treatment options in more detail and discuss their efficacy and potential side effects. Understanding the available treatments can empower healthcare professionals to provide the best care and support to individuals living with Alzheimer’s disease. 6. Providing care and support for individuals with Alzheimer’s Disease Next section: Providing care and support for individuals with Alzheimer’s Disease Caring for individuals with Alzheimer’s disease requires a compassionate and personalized approach. In addition to medical treatment, healthcare professionals play a crucial role in providing emotional support and guidance to both patients and their families. Creating a safe and comfortable environment is essential for individuals with Alzheimer’s. Simple modifications such as installing handrails, removing clutter, and labeling important items can prevent falls and promote independent living. It is equally important to encourage a regular routine and provide supervision as needed. Effective communication strategies are essential when caring for individuals with Alzheimer’s. Using clear, concise language and non-verbal cues can help facilitate understanding, while maintaining a calm and patient demeanor. Active listening and validation of emotions are also crucial in fostering trust and maintaining a positive relationship. Educating families about the disease’s progression and common challenges can alleviate anxiety and provide realistic expectations. Offering support groups, counseling, and connecting families with local resources can help them navigate the emotional and logistical aspects of caregiving. In the following blog
1. Introduction to Epilepsy: What is it and why is it important to understand and manage? Epilepsy is a complex neurological condition that affects millions of people around the world. Despite its prevalence, many misconceptions and stigmas still surround this disorder. Dr. Abhinav Gupta, a renowned neurologist specializing in epilepsy, has dedicated his career to improving the understanding and management of this condition. In this comprehensive guide, Dr. Gupta explores the various aspects of epilepsy, including its causes, symptoms, diagnosis, and treatment options. Whether you are a patient seeking answers or a healthcare professional looking to deepen your knowledge, this blog is an invaluable resource for anyone interested in exploring epilepsy. 2. Understanding the different types of seizures and their symptoms Understanding the different types of seizures and their symptoms is a crucial part of comprehending epilepsy. Epileptic seizures can vary in their presentation and severity, making it essential to recognize the distinctive features of each type. Generalized seizures, for example, affect the entire brain and can cause loss of consciousness and convulsions. Focal seizures, on the other hand, only impact a specific part of the brain, resulting in localized symptoms such as twitching or tingling. By understanding the specific symptoms associated with each type of seizure, individuals living with epilepsy and their caregivers can better manage and respond to these episodes. In the following section, we will delve deeper into the different types of seizures, their symptoms, and how they can be appropriately managed. Stay tuned to gain a more comprehensive understanding of epilepsy and its management. 3. Diagnosis and testing for epilepsy: What to expect If you suspect that you or a loved one may have epilepsy, it is essential to seek medical attention for a proper diagnosis. The diagnosis of epilepsy involves a thorough evaluation by a healthcare professional experienced in neurological conditions. During the diagnostic process, your doctor will conduct a detailed medical history, including discussing the symptoms and any possible triggers or patterns you have observed. In order to confirm the presence of epilepsy, your doctor may order a series of tests, including an electroencephalogram (EEG) which measures the electrical activity in the brain. This test is often performed during sleep or while the patient is in a state of sleep deprivation, as seizures can sometimes be more easily detected during these conditions. In some cases, additional tests such as brain imaging techniques like an MRI or CT scan may be recommended to identify any underlying structural abnormalities that may be causing the seizures. It’s important to note that the diagnosis of epilepsy can be complex and may require multiple tests and evaluations. However, these diagnostic measures are crucial in determining the most appropriate treatment plan for managing epilepsy effectively. In the next section, we will explore various treatment options available for epilepsy and how they can help individuals lead a fulfilling life. Stay tuned for more insights! 4. Managing epilepsy through medication and lifestyle changes Managing epilepsy involves a combination of medication and lifestyle changes to prevent and control seizures. Once a diagnosis is confirmed, your healthcare provider will work with you to develop an individualized treatment plan based on the type and frequency of your seizures. Antiepileptic medications are often the first line of defense in managing epilepsy. These medications help to reduce or eliminate seizures by stabilizing the electrical activity in the brain. It is important to take the prescribed medication as directed and report any side effects to your doctor. In addition to medication, certain lifestyle changes can also play a significant role in managing epilepsy. These changes may include getting enough sleep, reducing stress, avoiding triggers like flashing lights or certain foods, and maintaining a healthy diet and exercise routine. By closely following the prescribed treatment plan and making necessary lifestyle adjustments, many individuals with epilepsy are able to achieve seizure control and lead fulfilling lives. In the following section, we will delve deeper into specific medication options and lifestyle strategies for managing epilepsy effectively. Stay tuned for more information! 5. The role of healthcare professionals in epilepsy management When it comes to managing epilepsy, healthcare professionals play a crucial role in providing support, guidance, and expertise. From the initial diagnosis to ongoing treatment, they are there every step of the way to ensure that you receive the best care possible. First and foremost, it is essential to work closely with your healthcare provider to develop an individualized treatment plan. They will thoroughly evaluate your medical history, conduct necessary tests, and monitor your progress to determine the most effective course of action. They will also prescribe and adjust medications as needed, keeping a keen eye on any potential side effects. Regular follow-up visits with your healthcare provider are essential to evaluate the effectiveness of your treatment plan, make any necessary adjustments, and provide guidance on lifestyle changes. These professionals have extensive knowledge and experience in managing epilepsy and can offer valuable insights to help you navigate the condition. Furthermore, they can provide resources and recommendations for additional support services such as support groups, counseling, or educational programs. These resources can help you better understand your condition, cope with any emotional and psychological challenges, and connect with others who are going through similar experiences. Remember, you are not alone in this journey. Your healthcare provider is your partner in managing epilepsy, and together, you can work towards achieving optimal seizure control and a better quality of life. In the next section, we will delve deeper into different types of antiepileptic medications commonly prescribed to manage epilepsy. Stay tuned to learn more about how these medications work and their potential benefits and side effects. 6. Alternative therapies and treatments for epilepsy While medications are the most common method of managing epilepsy, there are alternative therapies and treatments that some individuals may consider. It is important to remember that these options should not be used as a replacement for traditional medical care and should always be discussed with your healthcare provider. One
Introduction Maintaining good mental health is essential for our overall well-being. It allows us to cope with the daily challenges of life, build resilience, and enjoy a fulfilling life. In this blog post, we will explore ten tips that can help promote good mental health. Let’s dive in! Food Eating a nutritious diet plays a crucial role in supporting our mental health. The food we consume directly affects our brain functions, mood, and energy levels. Here are some tips to keep in mind: Remember, small changes in your diet can make a big difference in promoting good mental health. Exercise Regular physical activity not only benefits our physical health but also has a profound impact on our mental well-being. Here are some exercise tips to boost your mental health: Social Connections Having meaningful social connections is vital for maintaining good mental health. Humans are social beings, and interactions with others provide a sense of belonging and support. Consider these tips: Building and maintaining strong social connections can significantly contribute to your mental health and overall happiness. Sleep Adequate sleep is often underestimated, but it plays a crucial role in our mental well-being. When we sleep, our brain performs essential functions that impact our mood, cognitive abilities, and overall mental health. Follow these tips for a restful night’s sleep: By prioritizing sleep, you allow your brain to recharge and support your mental well-being. Stress Management Managing stress is essential for good mental health. While it’s impossible to eliminate stress entirely, we can learn healthy coping mechanisms. Consider these tips: By implementing effective stress management techniques, you can help prevent the negative impacts of chronic stress on your mental health. Limit Alcohol and Drug Use Excessive alcohol and drug use can have a detrimental effect on our mental health. While they may offer temporary relief or relaxation, the long-term consequences can be damaging. Consider these tips: By limiting alcohol and drug use, you protect your mental health and reduce the risk of developing substance-related problems. Seek Support Remember, seeking support is a sign of strength, not weakness. Never hesitate to reach out for help if you’re struggling with your mental health. Here are some avenues to explore: You don’t have to face your mental health challenges alone—seeking support is a crucial step towards healing and well-being. Practice Gratitude Cultivating gratitude can have a profound impact on our mental health and overall outlook on life. By focusing on the positives, we shift our mindset and find joy in the simplest of things. Consider these tips: By incorporating gratitude into your daily life, you can nurture a positive mindset and boost your mental well-being. Disconnect and Recharge In today’s digital age, constant connectivity can take a toll on our mental health. It’s crucial to disconnect and give ourselves time to recharge. Consider the following tips: By disconnecting from the digital world, you create space to recharge and prioritize your mental well-being.
Epilepsy is a neurological disorder characterized by recurrent seizures, which are sudden bursts of electrical activity in the brain that temporarily affect how it works. Symptoms can differ greatly among individuals, primarily based on the type of seizures and the specific brain regions involved. Dr. Abhinav Gupta sheds light on some prevalent symptoms of epilepsy: Common Symptoms of Epilepsy FAQs About Epilepsy Symptoms: Q: Can you have epilepsy without having seizures? A: No, epilepsy is diagnosed based on the presence of recurrent seizures. Q: Are all seizures noticeable? A: No, some seizures, like absence seizures, can be very subtle and might go unnoticed. Q: Can seizures be prevented? A: While not all seizures can be prevented, proper treatment and avoiding known triggers can significantly reduce their frequency. Q: Do seizures cause permanent damage? A: Prolonged seizures, known as status epilepticus, can cause permanent damage. However, short, isolated seizures are less likely to have long-term effects. Conclusion: It’s crucial to understand that not every seizure is a sign of epilepsy. Other medical conditions, certain drugs, or withdrawal from substances can provoke seizures. Anyone experiencing new or recurring seizures should consult a healthcare professional. Epilepsy management often involves medication, lifestyle changes, and sometimes surgery. With proper care, individuals with epilepsy can lead full, active lives. For a more comprehensive understanding, or if you suspect you or a loved one may be exhibiting signs of epilepsy, it’s essential to consult with a healthcare provider for a thorough evaluation and personalized care plan.
You’re on a conference call and somehow wandered into the kitchen. Next thing you know you’re eating crackers and dry cereal out of the box. Or maybe you got so caught up.
Epilepsy is a neurological disorder that affects millions of individuals worldwide. It can have a significant impact on their daily lives, causing seizures and other associated symptoms. There are various causes of epilepsy, including genetic factors, brain injuries, infections, and brain tumors. The condition can be diagnosed through medical history assessment, neurological examination, and EEG tests. Treatment options for epilepsy include anti-epileptic drugs, a ketogenic diet, and surgical interventions. However, epileptic individuals can also manage their condition effectively through lifestyle changes, developing a seizure response plan, and seeking support from a network of healthcare professionals, family members, and friends. In this article, we will explore the causes, symptoms, diagnosis, treatment, and management of epilepsy, as well as its link with mental health. We will also provide answers to some frequently asked questions related to epilepsy. What is epilepsy? Epilepsy is a neurological disorder that affects the brain’s electrical activity, causing recurrent seizures. These seizures can vary in intensity, duration, and type, and can occur spontaneously or triggered by specific factors. During a seizure, the brain’s normal electrical activity becomes disrupted, resulting in abnormal or excessive electrical impulses that can cause various physical and mental symptoms. Epileptic seizures can affect different parts of the brain, leading to different types of seizures. Common Causes of Epilepsy Epilepsy can develop in individuals of all ages and backgrounds. While the exact cause of epilepsy is unknown in many cases, there are several factors that can contribute to the development of the condition. Cause Description Genetics Family history of epilepsy can increase the risk of developing the condition. Certain genes may also make an individual more susceptible to seizures. Brain Injury Brain injuries caused by trauma, stroke, or other factors can damage the brain and increase the risk of epilepsy. Infections Infections such as meningitis or encephalitis can cause inflammation of the brain, leading to seizures and epilepsy. Brain Tumors Tumors in the brain can disrupt brain function and cause seizures, which can lead to the development of epilepsy. In some cases, the cause of epilepsy may be a combination of these factors. It is important for individuals with epilepsy to work with a healthcare professional to determine the underlying cause of their condition and develop an appropriate treatment plan. Symptoms of Epilepsy Epilepsy is a neurological disorder that affects the brain’s ability to function properly, and this disruption can lead to a wide range of symptoms. The most common symptom of epilepsy is seizures, which can take many forms and affect individuals differently. Seizures can range from mild to severe and can include loss of consciousness, confusion, convulsions, muscle spasms, and more. Some individuals may only experience seizures periodically, while others may experience them on a daily basis. In addition to seizures, individuals with epilepsy may also experience other symptoms, such as: Staring spells Difficulty speaking or communicating Sudden mood changes Loss of bodily control It’s important to note that not all seizures are indicative of epilepsy. Certain medical conditions and external factors, such as high fevers or drug use, can also cause seizures. If you or someone you know experiences seizures or any of these symptoms, it’s crucial to seek medical attention for a proper diagnosis. Diagnosis of Epilepsy Diagnosing epilepsy requires a thorough medical evaluation, including a detailed medical history assessment and neurological examination. The doctor will also perform an electroencephalogram (EEG) test to measure the electrical activity in the brain and detect any abnormalities that may indicate epilepsy. The medical history assessment will involve questions about the patient’s symptoms, family history of epilepsy, past medical conditions, and any medications currently being taken. The neurological examination will include tests to assess the patient’s motor, sensory, and cognitive functions. The EEG test involves placing electrodes on the scalp to record the brain’s electrical activity. It is a non-invasive procedure and typically takes around 30 minutes to complete. The results of the EEG test can help the doctor diagnose epilepsy and determine the type and severity of seizures the patient is experiencing. Treatment of Epilepsy Epilepsy is a chronic neurological disorder that can be managed through a range of treatment options. The most common treatment for epilepsy is anti-epileptic drugs (AEDs) which help control the electrical activity in the brain. These drugs are prescribed based on the type of seizures, the patient’s age, and medical history. In some cases, AEDs might not be effective, and the doctor may recommend other treatment options. Surgical interventions can be an effective treatment option for epilepsy, particularly when seizures are localized to a specific region of the brain. Surgery involves removing the affected area of the brain or disconnecting it from the rest of the brain. In recent years, the use of a ketogenic diet has shown promising results in reducing the frequency and severity of seizures. This diet is high in fat, low in carbohydrates and protein, and can be effective for some patients, particularly children. However, it is crucial to consult with a healthcare professional before starting a ketogenic diet. Treatment options for epilepsy Pros Cons Anti-epileptic drugs (AEDs) Effective in controlling seizures for most people with epilepsy May cause side effects such as drowsiness, dizziness, or mood changes Surgery Can cure epilepsy in some cases Risks associated with brain surgery, including infection, bleeding, and neurological deficits Ketogenic diet Can be effective in reducing the frequency and severity of seizures Requires strict adherence to the diet, which can be challenging for some people It is important to work closely with a healthcare professional to develop a personalized treatment plan that is effective for managing epilepsy. The choice of treatment depends on various factors, including the frequency and severity of seizures, the patient’s age and medical history, and the potential risks and benefits of each treatment option. Alternative and Complementary Therapies In addition to conventional treatments, some epileptic individuals consider alternative and complementary therapies, such as acupuncture, herbal medicine, and yoga. However, there is currently limited scientific evidence to support the effectiveness of these therapies in
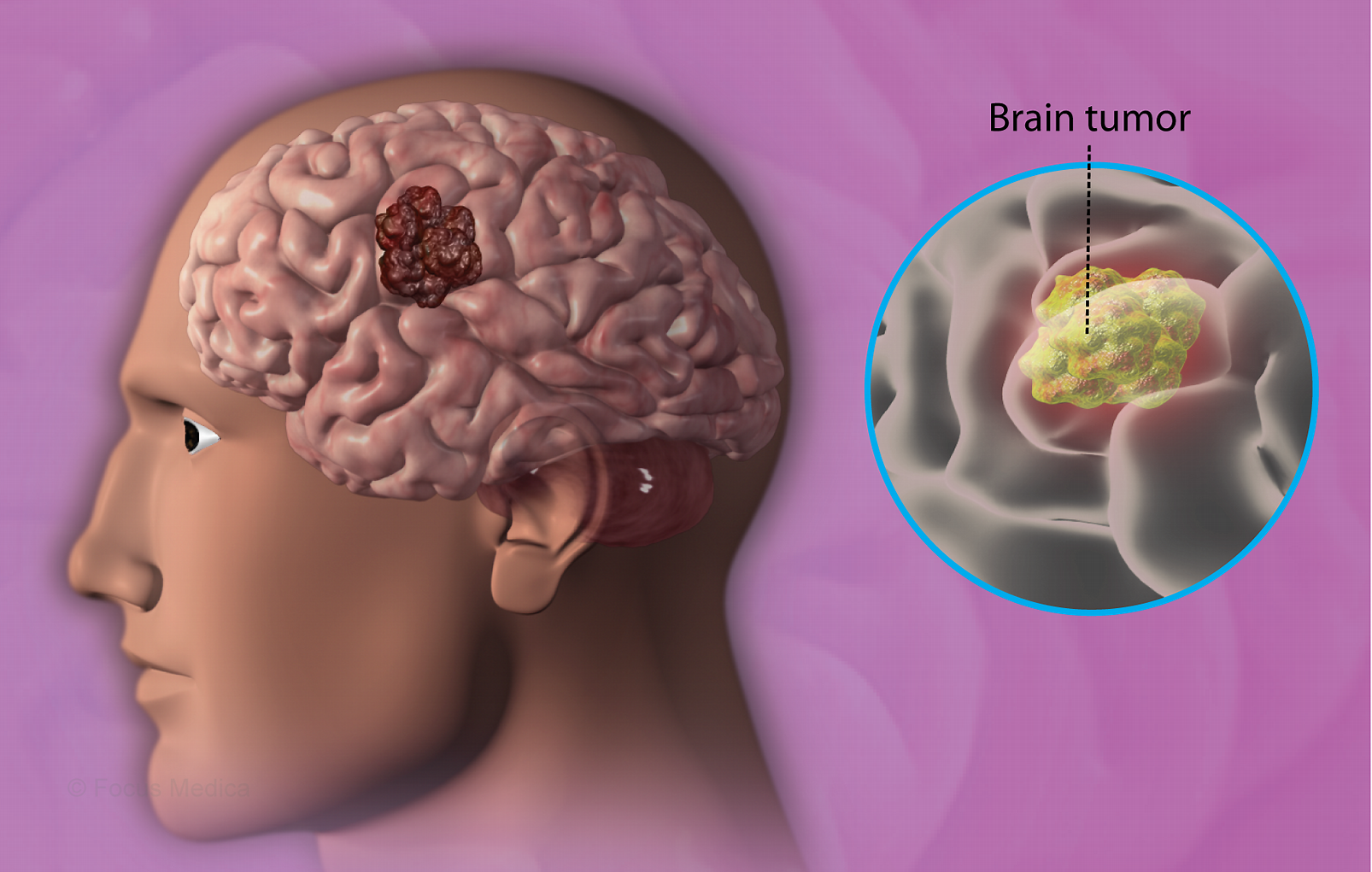
Welcome to our comprehensive guide on brain tumors. This article is designed to help you understand this condition and what you can do if you or a loved one are affected by it. Brain tumors can be scary and overwhelming, but by arming yourself with the right knowledge, you can take control of your health and make informed decisions about treatment. In this article, we will cover everything from the basics of what a brain tumor is and the symptoms to look out for, to diagnosis and treatment options. We will also discuss living with a brain tumor, prevention strategies you can use to reduce your risk and the latest research in the field. What is a Brain Tumor? A brain tumor is an abnormal growth of cells within the brain or the surrounding tissue. These tumors can be benign (non-cancerous) or malignant (cancerous), and can develop in any part of the brain or spinal cord. Malignant brain tumors are usually more aggressive and can invade nearby tissue, making them more difficult to treat. Types of Brain Tumors There are many different types of brain tumors, and they are classified based on the type of cell they originate from: Tumor Type Description Gliomas These tumors originate from the supportive tissue of the brain and can be either benign or malignant. Meningiomas These are usually benign tumors that grow from the meninges, which are the protective coverings of the brain. Acoustic neuromas These benign tumors develop on the nerves responsible for hearing and balance. Pituitary adenomas These benign tumors develop on the pituitary gland, which regulates hormone production. Metastatic tumors These tumors are not primary brain tumors but have spread (metastasized) to the brain from other parts of the body. The type of brain tumor can affect symptoms and treatment options, so it is important to have an accurate diagnosis. Brain Tumor Symptoms Brain tumor symptoms can vary depending on the type, size, and location of the tumor. Some people may experience no symptoms at all, while others may experience several. It’s important to note that having these symptoms does not necessarily mean you have a brain tumor, but they should be evaluated by a medical professional. Common Symptoms Some of the most common symptoms of brain tumors include: Headaches: Often worse in the morning or when lying down Seizures: Including convulsions and blackouts Changes in Vision: Blurred vision, double vision, or loss of peripheral vision Changes in Hearing: Ringing in ears, hearing loss, or sensitivity to sound Nausea or Vomiting: Especially in the morning or when changing positions Difficulty with Coordination: Loss of balance or trouble walking Changes in Mood or Personality: Irritability, confusion, or depression Less Common Symptoms In addition to the common symptoms listed above, there are several less common symptoms that can occur: Memory problems Speech difficulties Trouble with reading or writing Weakness or numbness in the arms or legs Difficulty swallowing If you experience any of these symptoms, it’s important to speak with a doctor. They can help determine if further testing is necessary to rule out a brain tumor or other condition. Brain Tumor Diagnosis Diagnosing a brain tumor typically involves a comprehensive medical evaluation. A doctor will begin by reviewing the patient’s medical history and symptoms, and then perform a neurological exam to assess brain function. This exam may include testing reflexes, muscle strength, memory, and coordination. If a brain tumor is suspected, the doctor may order one or more imaging tests, such as a magnetic resonance imaging (MRI) scan or a computed tomography (CT) scan. These tests can help visualize the tumor and provide information about its size, location, and characteristics. Diagnostic Testing Description Magnetic resonance imaging (MRI) Uses a powerful magnetic field and radio waves to create detailed images of the brain. Computed tomography (CT) scan Combines X-rays and computer technology to create detailed pictures of the brain. Angiogram Uses a contrast dye and X-rays to create images of blood vessels in the brain. In some cases, a biopsy may be necessary to confirm a brain tumor diagnosis. During a biopsy, a small piece of tumor tissue is removed and examined under a microscope. This can help determine the type of tumor and guide treatment decisions. It’s important to note that diagnosing a brain tumor can be a complex process, and it may involve multiple tests and consultations with various specialists. Patients are encouraged to ask questions and seek a second opinion if needed. Brain Tumor Treatment After a brain tumor diagnosis, there are several treatment options available. The best course of action will depend on the type, size, and location of the tumor, as well as the overall health of the patient. It’s important to discuss all options with a medical professional to determine the best treatment plan. Surgery Surgery to remove the tumor is often the first line of treatment for brain tumors. During the procedure, a neurosurgeon will remove as much of the tumor as possible while minimizing damage to healthy brain tissue. In some cases, the entire tumor can be removed. In others, some cancerous tissue may be left behind if it is too close to important areas of the brain. Radiation Therapy Radiation therapy uses high-energy beams to kill cancer cells. This treatment may be used alongside surgery or on its own for tumors that are difficult to treat surgically. Radiation therapy may cause side effects, including fatigue and memory problems, but they are usually temporary. Chemotherapy Chemotherapy uses drugs to kill cancer cells throughout the body. This treatment is usually reserved for advanced or high-grade tumors or when other treatments are not effective. Chemotherapy may cause side effects such as fatigue, nausea, and hair loss. Living with a Brain Tumor A brain tumor diagnosis can be overwhelming and life-changing. For those living with a brain tumor, it is important to take care of both physical and emotional health. Here are some strategies for coping with this condition: Find support: Connect with others who have gone
While most people who get COVID-19 are able to recover at home, the rush is on to find a treatment that’s safe and effective against life-threatening cases of the disease.
Migraines are more than just headaches; they are complex neurological events that can affect many parts of your life. Understanding the stages of a migraine can help in managing symptoms and seeking effective treatments. Migraine is a neurological condition that is characterized by recurrent headaches. It typically progresses through four stages: prodrome, aura, headache, and postdrome. The Four Stages of Migraine: 1. Prodrome (Pre-headache stage) The prodrome phase can serve as a warning sign that a migraine is about to occur. It can start hours or even days before the headache itself. This is the early stage of a migraine attack and can occur hours or days before the actual headache. Symptoms during this stage may include mood changes, food cravings, increased thirst, and frequent yawning. Some people also experience neck stiffness or heightened sensitivity to light or sound. 2. Aura Not everyone experiences the aura phase, but for those who do, it can be quite disconcerting. About one in four migraine sufferers experience an aura, which is a transient neurological disturbance. Auras often involve visual disturbances such as seeing flashing lights or zigzag lines, but can also affect other senses and motor functions. They usually last around 20 minutes to an hour and occur before or alongside the headache. 3. Attack Phase This is the phase when the actual migraine pain occurs and is often debilitating. This is the most well-known stage of a migraine attack and can last from a few hours to several days. The pain is typically throbbing or pulsating and can be accompanied by 4. Postdrome (Post-headache stage) Often referred to as a “migraine hangover,” this phase occurs after the headache subsides. FAQs: Q: Can migraines be prevented? A: While there’s no surefire way to prevent migraines, identifying and avoiding triggers, maintaining a healthy lifestyle, and following a preventive medication regimen (if prescribed) can help reduce frequency and severity. Q: Are migraines just bad headaches? A: No, migraines are complex neurological conditions. They involve various symptoms and stages and are more than just headaches. Q: When should I see a doctor for migraines? A: If you experience migraines frequently, if they are severe, or if they interfere with your daily life, it’s important to consult a healthcare provider. Q: Can children get migraines? A: Yes, children can experience migraines. Their symptoms might differ slightly from adults, and it’s important to seek pediatric care for proper diagnosis and treatment.
Parkinson’s disease (PD) is a neurodegenerative disorder that affects movement and is caused by the loss of dopamine-producing neurons in the brain. The exact cause of PD is not fully understood, but there are several factors that are believed to contribute to the development of the disease: Genetics: While most cases of PD are not directly inherited, there are certain genes that can increase a person’s risk of developing the disease. Mutations in the LRRK2, SNCA, and GBA genes are some of the most well-known genetic factors associated with PD. Age: Parkinson’s disease is more common in older adults, and the risk of developing the disease increases with age. Environmental factors: Exposure to certain environmental toxins, such as pesticides, herbicides, and solvents, has been linked to an increased risk of developing PD. Other factors, such as head injuries, may also increase the risk. Lifestyle factors: Certain lifestyle factors, such as a lack of exercise, a diet high in saturated fat, and smoking, may increase the risk of developing PD. Other medical conditions: Some other medical conditions, such as REM sleep behavior disorder and multiple system atrophy, have been linked to an increased risk of developing PD. Overall, the development of Parkinson’s disease is likely the result of a complex interplay between genetic, environmental, and lifestyle factors.